I want to start with some quotes from someone who has been leading the charge in raising awareness of the issues we are facing. Chris Kresser M.S., L.Ac. is the co-founder of the California Center for Functional Medicine, the founder of Kresser Institute, the host of the top-ranked health podcast “Revolution Health Radio,” the creator of ChrisKresser.com, and the New York Times best-selling author of The Paleo Cure and Unconventional Medicine. Mr. Kresser has so clearly stated:
“Our modern diet and lifestyle are out of alignment with our genes and biology. For most of evolutionary history, humans ate primarily meat and fish, wild fruits and vegetables, nuts and seeds, some starchy plants and tubers. Nobody ate processed food. There was no refined sugar, flour or seed oil. We went from a diet that was naturally anti-inflammatory, high in nutrients, and low in calories, to one that is pro-inflammatory, low in nutrients, and high in calories. This disparity is creating chronic pain, sickness and dysfunction in our society.”
“Our medical paradigm is not well-suited to tackle chronic disease. Conventional medicine is structured to address trauma, acute infection, and end-of-life care, not to keep people healthy. If you’re in a car crash and break your leg, the medical system is great to help you get your leg x-rayed, get your bones reset and get a cast on your leg so that it will heal properly. But most of us are using the healthcare system for less acute and more chronic conditions, and we can be frustrated by the lack of results.”
“Further doctors are trained the ‘expert model’ of simply telling people what to do, and expecting them to it – which is problematic considering they are not given enough time for patient appointments. To make things worse, doctors are expected to solve complex problems in impossible time frames and they are not trained to work collaboratively. Add in the fact that pharmaceutical companies control most of the information fed to doctors, and the picture starts to take hold. Without the right processes, and without much choice, the result is that primary treatment for 90% of all chronic conditions is pharmaceuticals. Almost 1/3 of adults take 2+ drugs. 30% of all teens are now on prescription drugs.”
“Our model for delivering care does not support the interventions that would have the biggest impact on preventing and reversing chronic disease. At one time, it seemed that genetics would hold the key to solving chronic disease. Recent studies have found that the majority of the risk of chronic disease is not genetic, but environmental and behavioral. Our genes do play a role in determining which diseases we’re predisposed to developing, but the choices we make about diet, physical activity, sleep, stress management, and other lifestyle factors are far more important determinants of our health.”
The US healthcare system is often described as fragmented, with various stakeholders (e.g., insurance companies, hospitals, and physicians) operating independently of one another. This leads to confusion and inefficiencies in the delivery of care. It also constantly creates a moving target for what success is, and these goals often are in conflict. Hospitals are trying to maximize their profits, so they increase prices and bureaucracy to deal with insurance companies that are trying to avoid paying money and minimize what they pay.
This is not the fault of doctors in general. It is a byproduct of a system with misaligned incentives and broken payment methods. Insurance goals and profit models are not always aligned with patient or doctor needs. And there is little incentive for healthcare providers to prioritize quality, efficiency, and cost-effectiveness in their approach. Most doctors can only spend 10-12 minute visits, some as few as 8 minutes. It’s impossible to deliver high-quality care in this limited time frame, especially if the patient has multiple chronic health problems, is taking several medications, and presents with new symptoms. And it leaves no time to dig into the diet, lifestyle, and behavioral areas, which are more likely the cause. Add to the fact that doctors have little to no training or understanding of these variables.
The result is a lack of emphasis on patient-centered care. The US healthcare system often prioritizes the needs of healthcare providers and organizations over those of patients. This leads to a lack of patient-centered care, contributing to lower quality of care and worse health outcomes.
And because so much of healthcare is now a battle for money between the hospitals, the government, and insurance companies, the system has evolved into an inefficient bureaucracy with extensive paperwork and administrative tasks required for many medical procedures. This can lead to delays in care and increased costs. And once again, a focus away from the actual patient care.
Sadly, a lot of this has been caused by lobbying by insurance companies and big pharma. It is resulting in political gridlock. Healthcare policy is often highly politicized in the US, with little agreement between political parties on addressing the healthcare system’s challenges. This can make it difficult to pass meaningful healthcare reform and contribute to instability and uncertainty in the healthcare market.
One of the most significant overarching issues is the overemphasis on profit. The US healthcare system is driven by profit, with insurance companies, hospitals, and pharmaceutical companies all operating for profit. This leads to a focus on generating revenue rather than improving patient outcomes. One of the most significant casualties of this is the “Standard of Care.”
The concept of “the standard of care” is often discussed among physicians, yet the legal definition of this term is frequently not understood. Emergency physicians are on the front lines of medicine and are frequently involved in medical malpractice cases. It is estimated that 7–17 malpractice claims are filed per 100 physicians every year.
The standard of care has evolved over the years and will continue to change as the legal theory in this area develops. The problem is that even lawyers do not know with certainty what it is. And while the general rule of thumb upheld most of the time is that the standard of care is what a minimally competent physician in the same field would do in the same situation with the same resources. So you can see how doctors, rather than serving their patients to their fullest capabilities, have to constantly be in fear of malpractice and an ambiguous standard of care.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3088386/
Thus, this ambiguity in the standard of care results in a lack of standardization, leading to variability in the quality of care and patient outcomes, even from one doctor to the next. And because there is a lack of transparency on pricing, quality, and standard of care, the system is difficult to navigate for patients and physicians as well. How can you make a well-informed decision about your healthcare and life if you cannot get transparency around pricing, quality of care, and medical outcomes?
While I am rarely an advocate of regulation since the industry is already highly regulated, in this case, it may be necessary. A major issue we are facing is higher healthcare costs. US healthcare costs are significantly higher than in other countries. This often results in patients delaying or avoiding necessary medical care. Even when they receive care, it creates exorbitant healthcare debt, which is one of the leading causes of bankruptcy in the US.
Unlike many other developed countries, the US also has high healthcare costs because it does not regulate the prices of medical procedures, drugs, and medical devices. A huge compounding factor is that people’s access to healthcare gets limited. Despite the Affordable Care Act (ACA), many people in the US still lack health insurance coverage, which can limit their ability to access healthcare when they need it. This is a segway to the next issue.
There is limited access to affordable insurance. The US healthcare system relies heavily on private health insurance, which can be expensive and unaffordable for many people. This can result in people going without insurance, delaying or foregoing necessary medical care, and incurring significant medical debt. Thus many people avoid treatments that could mitigate even great issues later on, resulting in more catastrophic medical issues over time for the patients and the system.
Another large issue is that as we moved away from holistic medicine, we moved towards allopathic medicine. Allopathic medicine focuses on alleviating the symptoms of the disease, while Osteopathic medicine is oriented to treating the patient, not the disease. Allopathic medicine or modern western medicine, refers to a system in which medical doctors and other healthcare professionals (such as nurses, pharmacists, and therapists) treat symptoms and diseases using drugs, radiation, or surgery.
A byproduct of this system is that it has moved away from the focus on primary and preventive holistic healthcare. Instead, it focuses more on specialized care. This often leads to higher costs and worse health outcomes, particularly for chronic conditions that could have been prevented or managed with early intervention. This focus leads to another major issue which is focusing too much on treating illnesses rather than preventing them in the first place.
While technology has paved the way for vast improvements and efficiencies in many industries, we have seen mixed results in healthcare. Fantastic advances in medicine have turned what was previously limited to the realm of science fiction into reality: we can restore sight to the blind, reattach limbs, and even clone human stem cells.
Our healthcare system has become overly reliant on technology. Remember that technology is often innovated and developed for profit, longevity, stability, etc. Not for health. For some treatments and procedures, this has provided significant advances. However, it has also led to substantially higher healthcare costs and a lack of emphasis on the human element of healthcare.
Software is often introduced to reduce the risk of file errors and redundancies. Redundancy is there to catch fraud, theft, and error. However, every digital medical record system, and especially the patient record management systems, have, rather than improved outcomes and doctor-patient visits, it hampered at best and perhaps decimated a struggling system by creating complex, difficult if not impossible to effectively use systems that have doubled if not tripled the time doctors have to spend on records for patient visits. It results in even less time for patient visits. This is also partially to blame for the increasing number of errors in medicine, as doctors are being required to increase their number of patient visits while also having to add the burden of these nightmare medical record systems.
Despite all these technological innovations, medical errors, such as misdiagnosis, medication errors, and surgical complications, are a leading cause of death in the US.
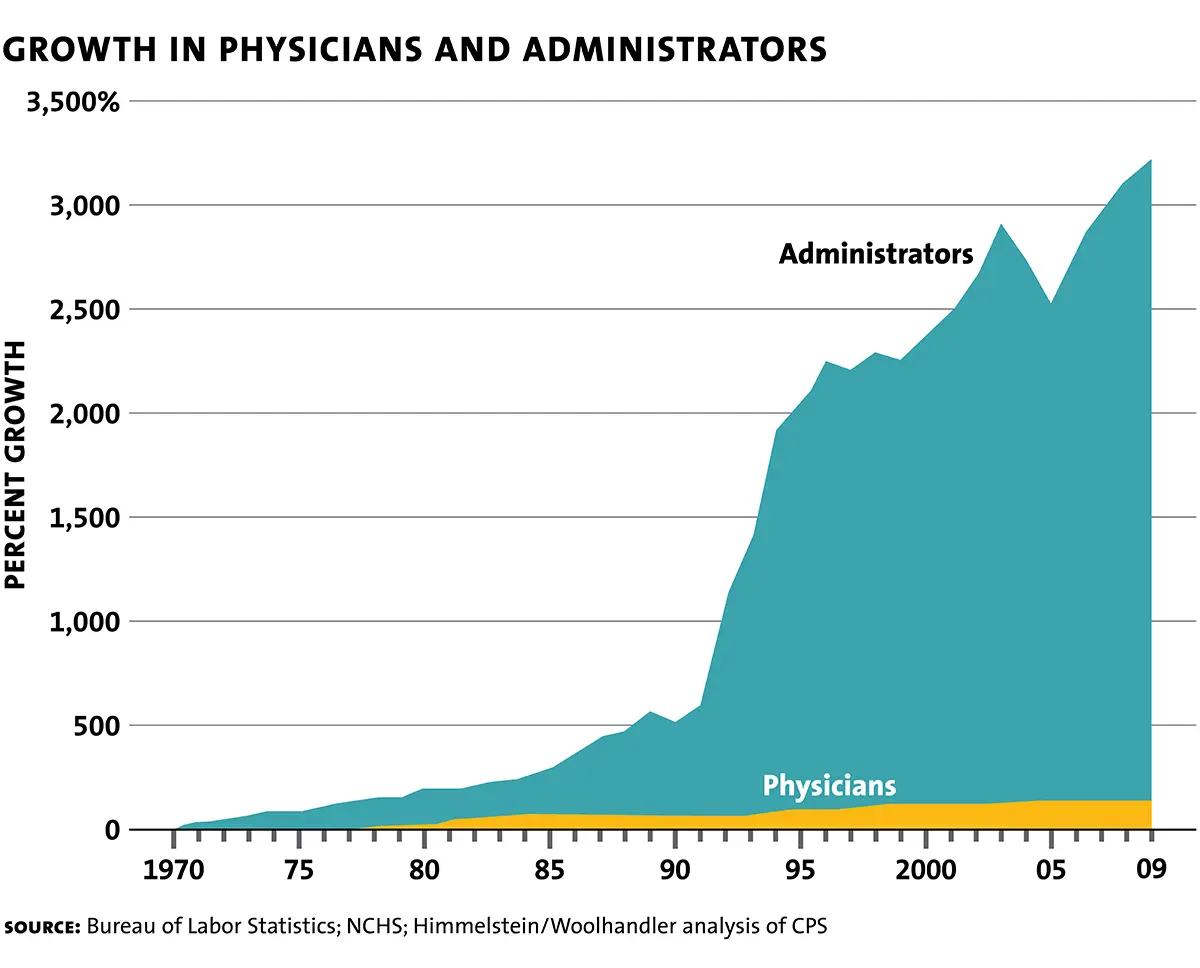
What’s more, it should come as no surprise that physicians are increasingly becoming burnt out. It is believed that as many as 60-70% of doctors struggle with burnout. Regardless of this or other factors as causes, we are now facing a growing shortage of physicians. While the number of administrators has increased, the number of doctors has stayed at a level that will likely drop off soon.
As we mentioned before, investors will always drive science. And outside of big pharma, medical research has recently stagnated in the US. Historically, the US has been a leader in medical research, but funding for that research has been in decline.
The treatments offered in conventional medicine are not necessarily the most effective or those supported by the most current evidence. Instead, they are the treatments that the insurance companies have agreed to reimburse. In other words, this is not evidence-based medicine, it is reimbursement-based medicine.
It would be inaccurate to call conventional medicine evidence-based. “It is simply no longer possible to believe much of the clinical research that is published,” says Marcia Angela, a former editor of the New England Journal of Medicine (Full Measure Staff 2016.)
To further complicate things, we must also keep in mind the influence of big pharmaceutical companies and their biases in research. The western medicine system was started by and funded for pharmaceutical companies. And while perhaps it was for originally good intentions, the focus now is on making money, over aligning patient and doctor needs. Nearly 2/3s of all research sponsored by pharmaceutical companies has led to conflict of interests, group think, and a failure to replicate many findings, undermining the credibility of the studies that form the edifice of our current medical paradigm.
With the focus of allopathic medicine primarily on big pharma-funded solutions, it should come as no surprise that in 2022 alone, big pharma revenues in the US alone were over $52 billion. When there is this much money to be made, and after the last chapter, you should be able to see that a major problem we face is the failure to adequately police and prosecute medical fraud in both treatments and research. The penalties to dissuade big pharma from causing harm are insufficient. It is more profitable and better for big pharma to kill people and just pay the fine later.
Here are some examples. The settlement amount includes both the civil (False Claims Act) settlement and the criminal fine. Glaxo’s $3 billion settlement included the largest civil False Claims Act settlement on record, and Pfizer’s $2.3 billion ($3.5 billion in 2022) settlement, including a record-breaking $1.3 billion criminal fine. Legal claims against the pharmaceutical industry have varied widely over the past two decades, including Medicare and Medicaid fraud, off-label promotion, and inadequate manufacturing practices. With respect to off-label promotion, specifically, a federal court recognized off-label promotion as a violation of the False Claims Act for the first time in Franklin v. Parke-Davis, leading to a $430 million settlement. If you want to see more, you can see the 20 largest settlements reached between the United States Department of Justice and pharmaceutical companies from 1991 to 2012.
https://en.wikipedia.org/wiki/List_of_largest_pharmaceutical_settlements
Fortunately, a big piece of the puzzle about why our medical system is failing us is also the piece you have the most control over patient education. Unfortunately, most people in America lack the knowledge and skills to manage their health effectively. It can be overwhelming and confusing, from diet to lifestyle to exercise. But it is also a set of levers you can control. The amazing thing is that if you take ownership of these variables, you can greatly mitigate your risks for poor health outcomes, unnecessary medical procedures, and higher healthcare costs. And that is why I wrote this book. In the following few sections, we will lightly go into some levers that you can take control of and greatly mitigate the risks to your health.
Or, if you want to read more about this topic, here is a great article.
https://doctorlib.info/health/unconventional-medicine/5.html

